The U.S. postpartum market currently generates $2.78 billion and is projected to more than double to $5.64 billion by 2035. As healthcare continues to move into the home, Let Mommy Sleep, with 15 years of trusted expertise, is uniquely positioned to bring postpartum and newborn services into the mainstream. Add newborn & postpartum care to your existing business to easily create a secondary stream of income and create a unique opportunity for caregiver recruits.

Why Add Newborn & Postpartum Care to Your Existing Business
Let Mommy Sleep newborn care and postpartum services are a proven way to unlock a profitable secondary stream of income. We deliver qualified, ready-to-book families directly to your inbox, therefore saving you time and cost on marketing outreach. Your agency can start generating revenue immediately with minimal overhead.
Because night nanny care and postpartum visits are private pay, your agency gains access to revenue that is both predictable and simple. Families pay directly for care, creating faster cash flow and higher margins. This new line of business also adds stability to your bottom line and protects against fluctuations in traditional healthcare funding.
Add Newborn & Postpartum Care to Your Existing Business to Increase Recruiting & Retention
Recruiting and onboarding is a pain point for just about every company, but especially in home health. Add newborn & postpartum care to your existing business and you’ll see:
- With diverse professional opportunities, your business stands out among qualified applicants
- As a result, caregiver retention rises when your workforce has more dynamic opportunities
- Opening up employment to infant caregivers widens your own pool of recruits
The newborn and postpartum market is an untapped opportunity for most home health agencies. By expanding into care for babies and parents, you capture a high-demand sector with built-in trust and urgency. Offering overnight newborn care and postpartum support not only differentiates your agency from competitors but also positions you as a full-spectrum healthcare provider. With Let Mommy Sleep, you don’t just add services, you expand into a lucrative, growing market that drives long-term business growth.
How It Works
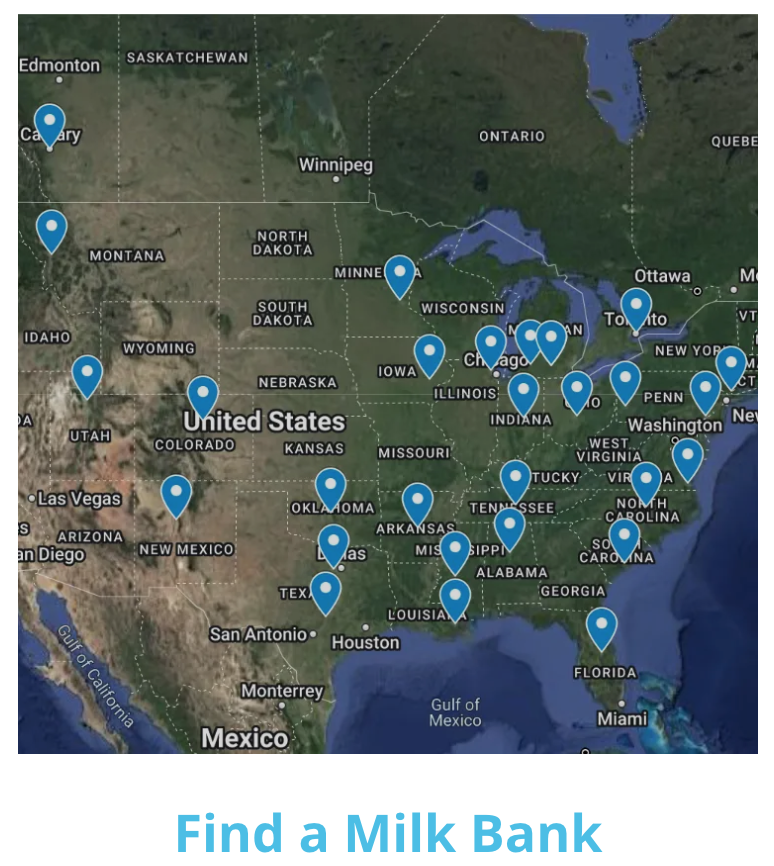
Licensing with Let Mommy Sleep is simple and cost effective. You can license monthly to “try before you buy” or yearly if you prefer. Your territory is also protected and divided by county, not zip code therefore giving you the greatest chance to succeed. You can learn more about our national brand here.
Contact us today to learn more.