Most recently updated, 10/26/2025
What You’ll Learn:
- Why and how newborns sleep differently than adults
- Week by week breakdown of baby’s expected time awake and asleep
- Understand when baby should be placed down for a nap.
Baby Sleep: Naps Decoded – Understanding Sleep Cycles
Newborns and infants sleep differently than adults. Once you understand why, you can work with their natural rhythms instead of against them, helping them sleep longer and with less fuss.
They’re tiny! – Newborns have small stomachs so they need to eat frequently. Their tummies can only hold small amounts of breast milk or formula and this nutrition gets digested quickly. As a result, they typically wake every 2 to 3 hours to feed. See the chart at How big is a newborn’s stomach?
Hunger, need for comfort or growth spurts – Babies usually wake up if they’re hungry, have a wet or dirty diaper, or are experiencing discomfort due to issues like teething or gas. Additionally periods of growth mean their bodies and brains are developing rapidly, leading to more frequent waking during the night.
Immature sleep patterns: Newborns have an immature sleep-wake cycle, and it takes time for their circadian and ultradian rhythms to develop. This means that their sleep is not yet regulated by day and night patterns, and they have shorter sleep cycles compared to adults.
Melatonin isn’t Present Yet: Newborns receive melatonin, widely known as the sleep hormone, from the placenta but don’t start developing their own until they’re about 8-9 weeks old.

Baby Sleep: Naps Decoded – Circadian Rhythm
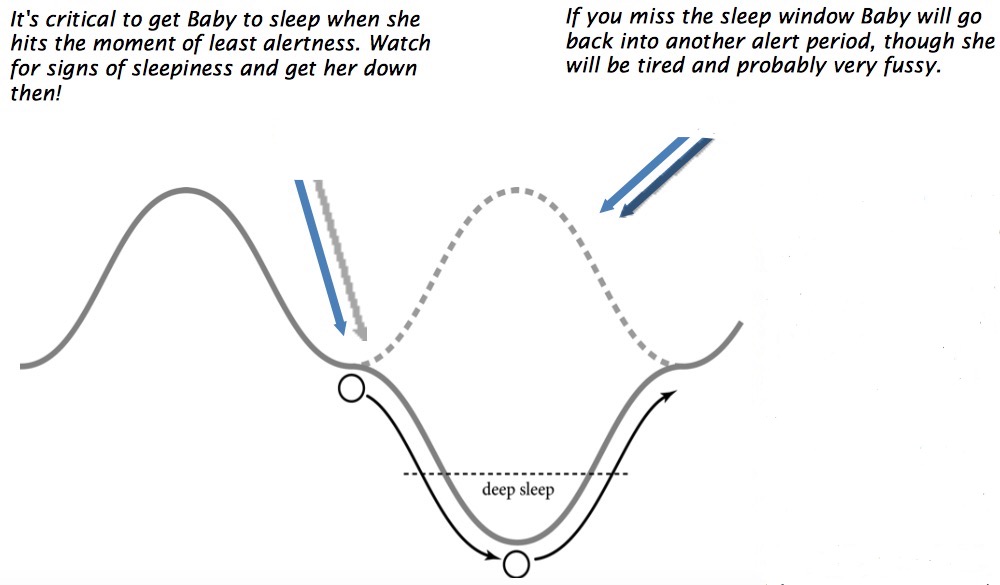
Circadian rhythm is nature’s 24-hour clock that regulates awake and sleep times. Within this cycle are shorter ultradian rhythms, lasting about 30–90 minutes, that dictate when babies move from alertness to sleepiness.
Every baby book about “schedules” or “wake windows” is based on these patterns—but let’s simplify how they actually work.
Ultradian Rhythm Basics
- Serotonin increases alertness and is triggered by daylight.
- Melatonin promotes sleepiness and is triggered by darkness.
If we visualize this using a 6-month-old as an example: baby is wakeful at the top of the curve (around 45 minutes after waking), and sleepy at the bottom (around 90 minutes after waking).
Tip: Put baby in the crib 5–10 minutes before that 90-minute mark—right before the “clock dings” and they become alert again.
In full-term newborns, melatonin production doesn’t mature until 9–12 weeks, so they build up to that 90-minute cycle gradually. Getting baby down before they enter another wakeful period prevents fussiness and overtiredness.
Nap Timing Reminder
Baby shouldn’t start winding down at the :30, :45, :60- or 90-minute mark. They should already be in their crib by that point.
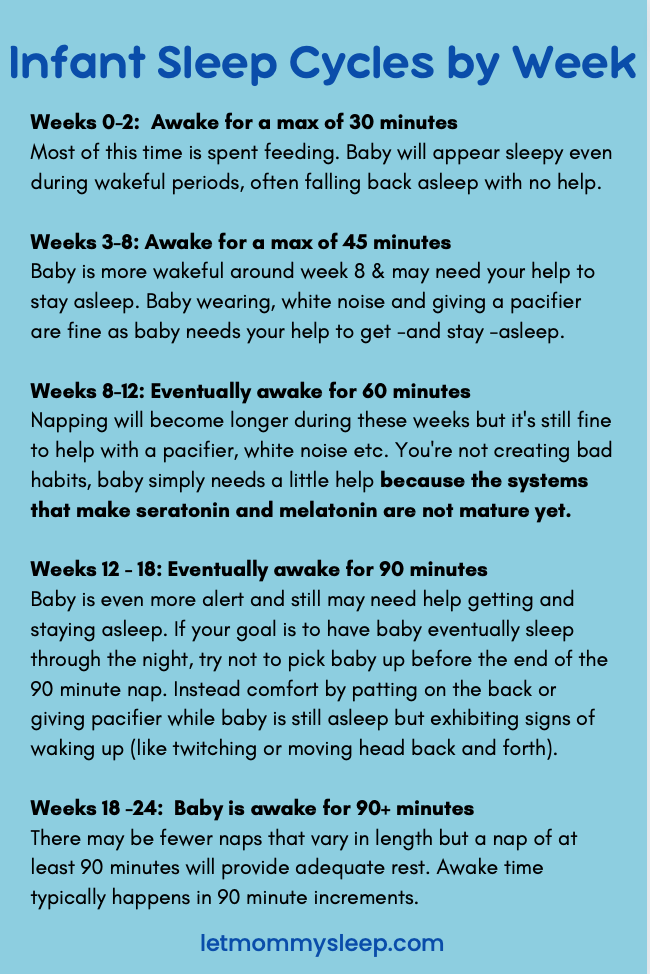
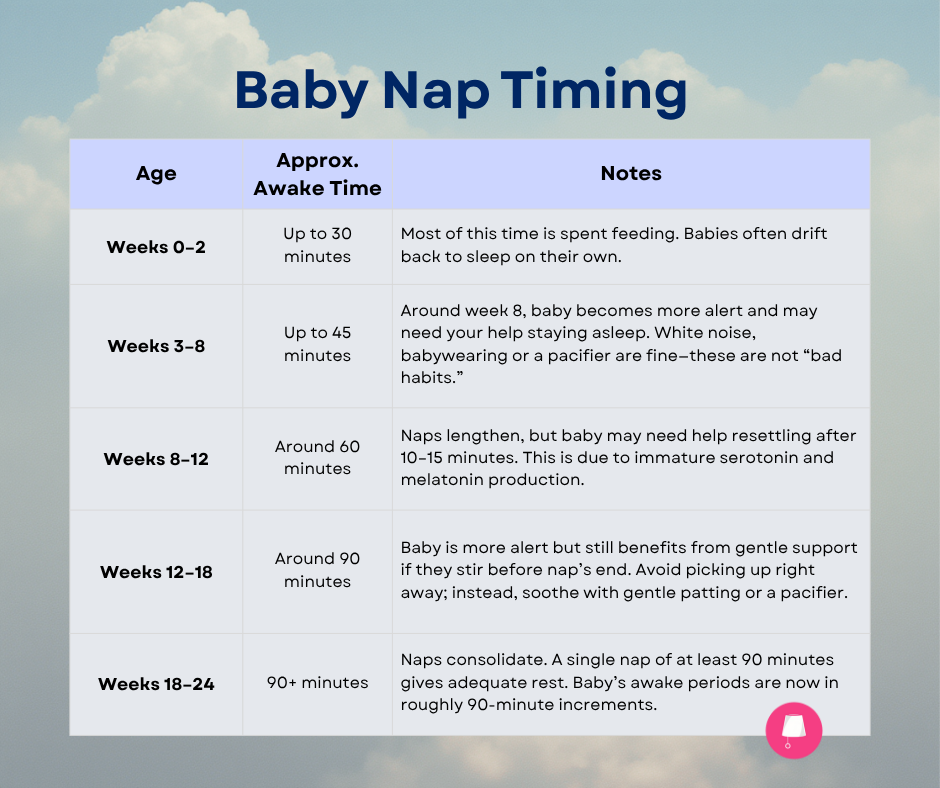
Here’s a breakdown of newborns’ basic awake and sleep times:
Baby Sleep: Naps Decoded
- Weeks 0-2: Baby is awake for a maximum of 30 minutes. Most of this time is spent feeding and baby will appear sleepy even during wakeful periods, often falling back asleep with no help at all.
- Weeks 3-8: Baby is awake for a maximum of 45 minutes. You’ll notice baby is more wakeful around week 8; s/he won’t just go right back to sleep like s/he used to and may need your help to stay asleep. Baby wearing, white noise, giving a pacifier to help sleep are all fine to do because at this age baby needs your help to get and stay sleep.
- Weeks 8-12: Baby is working on and eventually awake for 60 minutes. Napping will become longer during these weeks as well but it’s perfectly fine and even recommended to help baby with napping when s/he pops up after 10-15 minutes or so by giving a pacifier, using white noise etc. You’re not creating bad habits, baby simply needs a little help to not fully awaken because the systems that make seratonin and melatonin are not quite mature yet.
- Weeks 12 – 18: Baby is working on and eventually is awake for 90 minutes. Baby is even more alert and still may need help getting and staying asleep. If your goal is to have baby eventually sleep through the night independently, try not to pick baby up if she wakes before a 90 minute nap is done. Instead, stay near to comfort with patting on the back or giving pacifier while baby is still asleep, but exhibiting signs of waking up like twitching or moving her head back and forth.
- Weeks 18 -24: Baby is awake for 90+ minutes and consolidates naps now. There may be fewer naps that vary in length but a nap of at least 90 minutes will provide adequate rest. S/he will usually be awake for some increment of 90 minutes (11⁄2 hours, 3 hours, 4 1⁄2 hours).
What’s Next?
If your goal is to have baby sleep long stretches overnight without feeding, the 4 month well check is a great time to start talking with your pediatrician. These longer stretches of sleep are really just one big nap consolidation! They can help you to know whether baby is developmentally ready to sleep for at least 6 hours uninterrupted.
If you’re ready for your baby to sleep through the night, start with an appropriate routine. While the cry-it-out method gets a lot of press, sleeping through the night can be a gradual process where baby’s body adjusts to less milk overnight, making sleep a natural next step to waking from hunger. You can read about this in detail in the Ultimate Guide to Baby Sleep Training.
Baby Sleep: Naps Decoded – Important Notes
Sometimes even though we’re doing everything right, babies cry. A LOT.
They might cry because of colic, could be overstimulation, reflux or any other reason only known to your baby. Even if you follow this blog or any sleep advice exactly as it’s written, babies are not robots. You’re doing a great job. If you’re concerned about baby’s crying or health, please contact your pediatrician.
These guidelines are for full-term babies without medical concerns. Preemies, twins, and babies with special feeding or growth needs may follow different patterns. Some babies need to be woken for feeds to gain weight, for example. When in doubt, trust your instincts and your doctor. You can never go wrong with patience, following doctors’ orders and responding to your baby’s needs.
If you’re expecting and want more tips, visit Your First Week Home with Baby: Ultimate Q&A, by our Night Nurse (RN) and Night Doula team. Let Mommy Sleep team members are dedicated to safe sleep and evidence-based care, you can learn about this in Introducing the National NAPS Registry for Night Doulas.