Four Month Sleep Regression Explained- reviewed by Pam Jones, RN, 25+ year postpartum nurse and sleep coach, updated 8/16/2025.
The 4-Month Sleep Regression Explained in 30 Seconds
Newborns only go through 2 stages of sleep, but at 4 months old begin maturing into the 4 stages of sleep that we keep for the rest of our lives. The two new stages include lighter sleep. The 2 new stages mean more frequent night wakings and shorter naps. This is because for the first time in baby’s whole life, it’s easier for them to get woken up and they don’t yet know how to get themselves back to sleep.
During this time, many parents report that naps that used to be consistent suddenly shrink from 90 to 30 minutes, or that their baby starts being wide awake every 2 hours again. These changes can seem like baby’s sleep is taking a step backward, but they’re actually signs that your infant’s sleep cycles are maturing.
It’s a normal progression that happens before your baby is able to sleep longer stretches overnight. It can be frustrating but knowing why and when it’s happening, and being prepared to ease the transition can help. Sticking to consistent routines, using soothing techniques like a pacifier and trying to let your baby fall asleep independently can all help with the transition to more mature sleep.
The 4 Stages of the Sleep Cycle
In order to understand how your full-term baby is developing with regard to sleep around four month’s old, we first need talk about sleep in general.
Many of us just think of sleep as an on-or-off situation. You’re either asleep or you’re not. But sleep actually has a number of different stages that make up the “sleep cycle.” Starting at 4 months old, the brain matures into going through all 4 of the stages several times a night and this is the cycle we use for the rest of our lives.
- Stage 1 is that initial stage we’re all familiar with where you can just feel yourself drifting off, but don’t really feel like you’ve fallen asleep. In this stage, you could still hear your name if someone called you and it’s very easy to wake up.
- Stage 2, considered the first “true sleep” stage. This is where people tend to realize, once woken up, that they actually were sleeping.
- Stage 3 is deep and regenerative. Also known as “slow wave” sleep, this is where the body starts repairing and rejuvenating the immune system, muscles tissue, energy stores, and sparks growth and development.
- Stage 4 is REM (rapid eye movement) sleep. This is where the brain starts to kick in and consolidates information and memories from the day before. It’s also the stage where we do most of our dreaming.
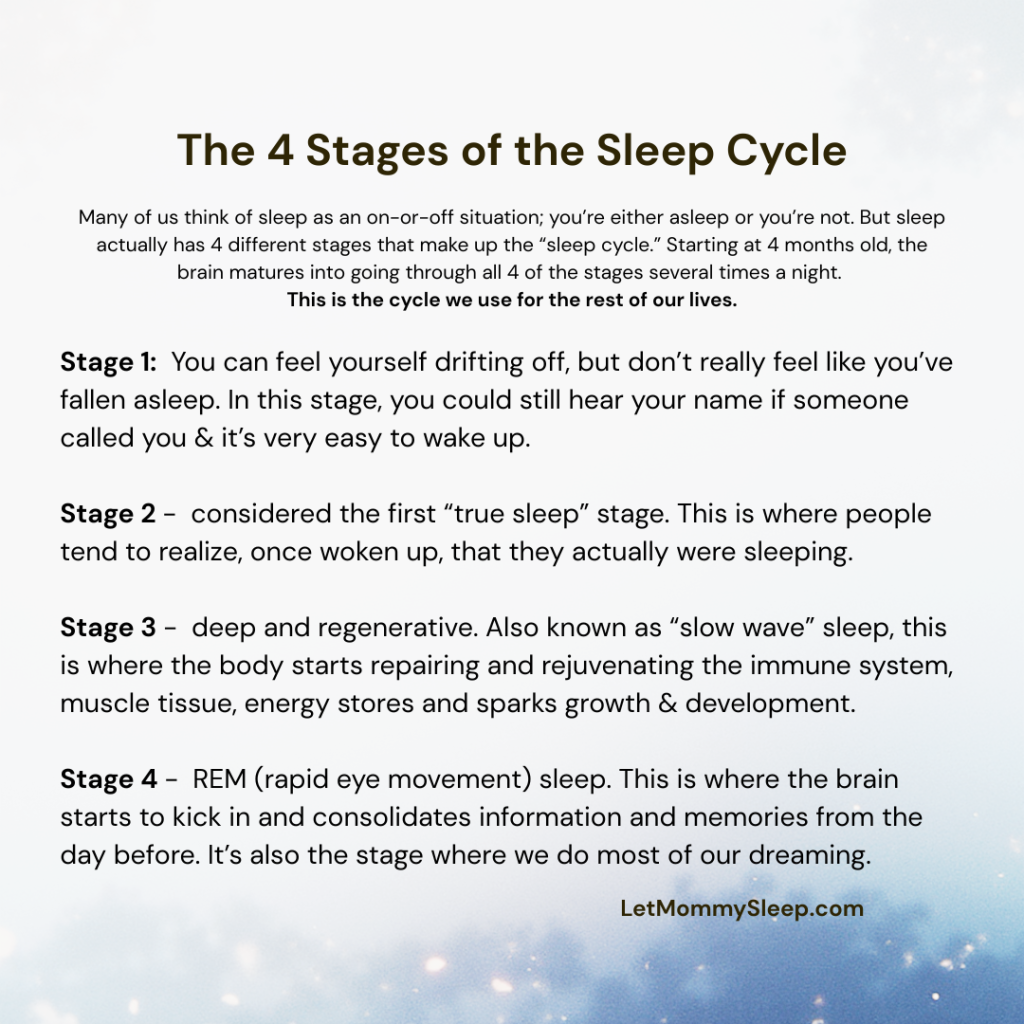
Once we’ve gone through all of the stages, we either wake up, or come close to waking up, and then start over again until morning.
Sleep from Newborn to 4 Month’s Old
Newborn babies only have 2 stages of sleep; stage 3 and REM. They spend about half their sleep in each stage. At around the third or fourth month, there’s a reorganization of sleep, as they embrace the 4-stage met.hod of sleep described above. And as the AAP notes, babies don’t have regular sleep cycles until about 4 months of age
When the change to the 4 stage method of sleep takes place, baby moves from 50% REM sleep to 25%, in order to make room for those first two stages. Although REM sleep is light, it’s not as light as the 2 new stages of sleep they’re getting used to. With more time spent in lighter sleep, there’s more of a chance that baby will wake up.
Waking up is absolutely natural, and we continue to wake up three, four, five times a night into adulthood. As adults however, we’re able to recognize that we’re in bed and safe and we go back to sleep. This usually happens so quickly that we don’t even remember in the morning.
For a four-month old infant though, these types of wake-ups are something they’ve never experienced before in their whole life! So it makes sense that they need our help to get back to sleep. Whether they’re usually rocked back to sleep, need a pacifier or just need reassurance, your baby most likely will not go back to sleep without your help, and a normal bedtime routine includes your help at this point. (Mayo Clinic)
How to Get through the Four Month Sleep Regression
Other contributor to infant’s waking up more often overnight, is that their “normal” is facilitating sleep with a pacifier, by being rocked or by being breastfed. Let me say this part in all caps though: getting baby to sleep these ways are ALL NECESSARY, NORMAL AND NOT “BAD HABITS.”
To get through the 4 month sleep regression, or any sleep disturbances you can:
- Use a pacifier – At 4 months, more time is spent in light sleep with higher probability of waking up. If you’re baby is used to a pacifier, be ready to replace the paci multiple times per night since they’re still too small to do it.
- Keep the room dark – Newborns and infants are not afraid of the dark. They are however, responsive to light. Light tells our brains that it’s time for activity and alertness, and the brain secretes hormones accordingly, so we want to keep the sleep area darkened, eliminating sunlight and possible flashes of light during naps and bedtime.
- …and use white noise – The other nemesis of sleep is noise. With more time spent in lighter sleep, noises can startle baby awake so white noise is a great addition to your nursery.
- Instill a bedtime routine – Bedtime routines should be about 20 – 30 minutes long, and baby should go into their crib while they’re still awake. Feeding should happen first, with whatever calm activity baby likes second and then a diaper change and PJs at the end.
Sleeping through the Night and the Four Month Sleep Regression
If your goal is sleep training after 4 months, when the pediatrician agrees it’s appropriate for baby to sleep long stretches, you’ll need to instill a new part of the bedtime routine to replace the milk = sleep association. Here’s what that means:
- Offer breast or bottle when your baby wakes for the day and after naps. Babies are naturally hungry then of course, and feeding while they’re most alert gives their bodies plenty of time to digest before the next sleep.
- Include a feed at the start of the 20-30 minute bedtime routine. This way the bottle isn’t the last step before sleep and baby will not be using milk as their tool to getting to sleep. Feeding at the beginning of the wind down routine also guarantees you a diaper change, and a clean diaper right before baby goes down for the night.
- If baby always falls asleep while feeding, they’ll associate bottle or breast with sleep, making it harder to learn how to fall asleep on their own.
Note: With newborns, you can’t prevent them from nodding off at the breast or bottle and that’s okay. RN Heidi explains this in The NoClock Nursing Method As babies get older, they naturally stay awake for feeds, which makes this routine possible.
Four month old infants typically go about two hours between snoozes, with bedtime between 7 and 8 at night. Once babies graduate from the four month sleep progression, they follow the sleep patterns they’ll have for the rest of their lives…four stages repeated multiple times a night! Of course, you may have to sleep train to fully help them sleep through the night if that’s something you want to do, the Ultimate Guide to Baby Sleep Training has step by step instructions.
Four Month Sleep Regression FAQ’s
1. How long does the 4-month sleep regression last?
Most babies experience this sleep disruption for 2 to 6 weeks. Once they adjust to their new sleep cycles nighttime sleep and naps gradually improve.
2. Is sleep training safe at 4 months?
Gentle sleep training can begin around 4 months for full-term, healthy babies but always check with your pediatrician first as babies’ developmental and physical readiness varies. Start by focusing on consistent routines that gradually wean feeding overnight rather than a “cry it out” method.
3. Can teething cause sleep regression?
Teething doesn’t cause an entirely new regression, but discomfort can worsen existing sleep challenges and cause waking overnight.
4. Should I feed my baby during night wakings at 4 months?
Many 4-month-olds still need 1–2 nighttime feeds, depending on weight and feeding history. With your pediatrician’s approval you can gradually lessening the amount taken at each feed to pave the way for falling back asleep independently.
5. When should I call my pediatrician about sleep issues?
If your baby’s sleep suddenly changes along with poor feeding, weight loss, or signs of illness, check in with your pediatrician. Persistent sleep problems beyond 6 weeks may indicate another issue worth evaluating.
This article was written with input and review from Pam Jones, RN. Pam has provided traveling in-home newborn and postpartum care for families since 2009. She has been a Registered Nurse for 25 years and is also a Sleep Consultant and Author of Raising Confident Parents: Secrets from Baby Nurses and Parents about Pregnancy, Infant Care, and Achieving Sweet Dreams. This article is for educational purposes only and does not replace medical advice. Always consult your pediatrician if you have concerns about your baby’s sleep.