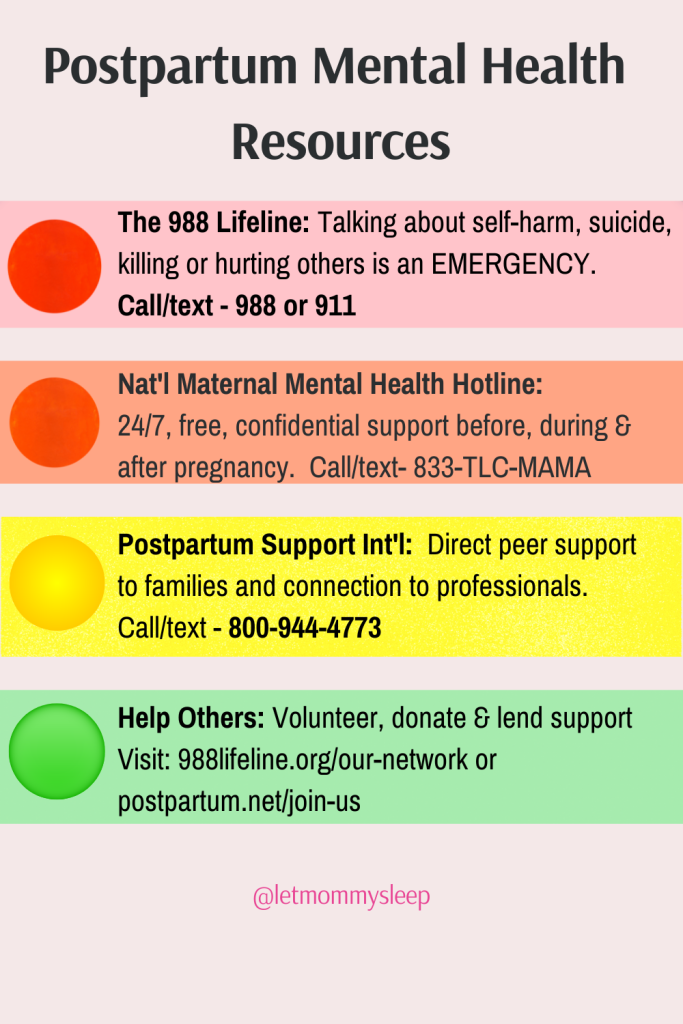
Updated February June 18, 2025 – Perinatal or postpartum mood and anxiety disorders, also called PMAD’s, are the most common complication of pregnancy. But unlike physical emergencies which are often obvious to us, it can be hard to know when to reach out for help. If you’re not sure what kind of support is needed, the Postpartum Mental Health Resources chart below can help.
Postpartum Mental Health Resources – An Overview
Emergency Resources
Below are postpartum resources in order of emergency need. Share and bookmark this resource.
- Emergency Level of Care: The 988 Lifeline – Talking about self-harm, suicide, killing or hurting others is an EMERGENCY. The Lifeline provides 24/7, free and confidential support for people in distress. Call or text 988 from any phone or visit 988lifeline.org
- Emergency Level of Care: 911 – 911 can always intervene when an emergency is present. The threat of hurting oneself or others is an emergency.
Non-Emergency Support
- Non emergency – but still very necessary! – support before, during and after pregnancy: The National Maternal Mental Health Hotline: Free, confidential support 24/7 during all phases of maternal need. Call/text 833-TLC- MAMA (852-6262). The hotline offers access to professional counselors, referrals to local and tele-health providers and support group connection. Interpreter services in 60 languages are available.
- Support Level during Postpartum Phase: Postpartum Support International – The organization provides direct peer support to families, trains of professionals, and provides a bridge to connect them. 800-944-4773.
- Helping Others – Have you come out on the other side of mental health distress and now want to help others do the same? Contact any of the organizations listed here to volunteer or donate.
Education Before Baby Arrives – Understand Mental Issues
Educate yourself and your loved ones about potential issues before baby arrives. A good rule of thumb is that if you or someone you love is having thoughts that scare you, it may be an emergency and help should be called. But what if you just feel “off”? Or your loved one doesn’t seem to be getting better? Become familiar with what’s normal versus what’s not to make the difference between a bump in the road and a crisis situation.
Here’s how you can get educated about postpartum mental health:
- Learn and Talk About It Before Baby Arrives: First, understand postpartum depression PPD vs. Baby Blues: Know the Difference. This can help you to see when typical postpartum behaviors such as weepiness or fatigue cross the line to becoming a mental health concern. This is different for everyone depending their usual demeanor, so it’s helpful to understand you and your partner’s baseline moods and if they change in the weeks after baby arrives.
Questions you can ask yourself if you feel normal baby blues are blurring into a mood disorder are: Do I seem more sad than happy? or Does my partner have anxious thoughts that were never there before?
- Assign an Advocate: Partners are usually each other’s advocates and first line of defense in addressing mental health. Learn the signs of postpartum depression vs. normal Baby Blues before baby arrives. If you don’t have a partner, ask a trusted loved one to specifically look out for your mental health. Visitors often ask about the baby, not the parent. The default answer is usually ‘Fine!’ — which is why having a trusted advocate to monitor your mental health is crucial. For this reason, parents should be on alert for changes in each other’s mood and behavior, or have a trusted love one taking on this role.
- Dads & Partners – Dads and non-birthing partners are at risk of Paternal PostNatal Depression. In fact, an NIH study notes depression can affect up to 25% of new fathers. Learn your own risks and bookmark resources like Postpartum Support Int’l that have specific tools for you.
- Family, Nannies & Caregivers – Building on the tips above, share these resources with those who can look out for you and your partner. In fact, many times when we’re in distress, others notice that we’re acting differently before we do.
- Understand Crisis Situations – It can be hard to know when to call a doctor or when to reach out for emergency help. If you’re unsure, Mara Watts, M.A., M., Ed. of Postpartum Support of Virginia has an excellent rule of thumb: “If you are having thoughts that scare you, this is an emergency.”
Postpartum Mental Health Resources – Keep going
Postpartum depression can present for up to a year after baby’s birth. For ongoing mental wellness, local support groups are often free or very low cost:
- MOMSClub.org, which stands for Mothers Offering Mothers Support – These are community based organizations that have groups based on zip code, so the parents in the group are your neighbors too!
- Parents of twins and higher order multiples might also find their local village at Multiples of America.org
- You local hospital very likely has a New Parents Postpartum Meet up
- La Leche League is also free and supports all parents.
Whatever level of support is needed, there is help for you. Please let us know if we can help connect you with these resources or provide overnight support to help you recuperate or get healthy. Mental and physical wellness depend on each other!
Are you expecting or want to be proactive about postpartum mental health resources? Bookmark Your First Week Home with Baby: Ultimate Q&A