Postpartum recovery doesn’t look the same for everyone. If you can’t or choose not to breastfeed, you may be wondering what changes to expect in your body and how to take care of yourself in the weeks after birth. Your body will still go through hormonal shifts, breast changes and physical healing and Postpartum Recovery: What if You’re Not Breastfeeding? aims to make the transition smoother to help you focus on rest, healing and bonding with your baby.

Breast Changes if You’re Not Breastfeeding
Nursing or not, your breasts may still become swollen, tender, or engorged around day 3–5 postpartum. This is normal and gradually subsides within 1–2 weeks.
Q: How can I get my milk to dry up If I’m not breastfeeding?
- Wear a supportive, snug bra without underwire to minimize irritation and stay comfortable. A sports bra or compression bra give gentle support while allowing milk to gradually reabsorb and production to slow down. The focus is on comfort and reducing stimulation so your body knows that milk isn’t needed.
- Use cold compresses or chilled cabbage leaves to reduce swelling.
- Hand-express only enough to relieve discomfort; avoid fully emptying breasts to prevent prolonging milk production. Breastmilk is produced on a supply and demand basis, so when emptying the breasts you don’t want to increase demand.
Q. What’s Cabergoline?
Cabergoline is a simple, effective and generally safe medication that suppresses lactation. Cabergoline is a tablet that works by stopping your body’s production of prolactin, the hormone that helps maintain milk supply. While only 1 dose is typically prescribed, side effects of dizziness, headache or bloating may occur.
Physical Recovery and Hormone Shifts
Postpartum physical and hormonal changes will happen regardless of your feeding choice. Estrogen and progesterone fluctuate and this can lead to mood swings or fatigue. To manage your hormonal health be sure to stay hydrated and eat nutrient-rich meals, rest when you can and track your mood to to self-screen for postpartum depression.
Physical recovery will be directed by your maternal healthcare team but in general, these home remedies aide in healing and pain management:
- Over the counter pain relief such as ibuprofen if cleared by your doctor
- Use of ice packs or sitz baths for perineal discomfort. Sitz baths are simply warm bathwater with a small amount of salt added that you can sit in for 10-20 minutes.
- Begin gentle pelvic floor exercises once cleared by your healthcare provider to support your bladder, bowel and uterus.
- Supporting your body with nutrition and light activity is also important for energy and recovery.
Postpartum Recovery: What if You’re Not Breastfeeding – Call your OB/GYN or midwife if you experience:
- Severe breast pain, redness, or warmth. This can indicate possible mastitis which is internal inflammation, often accompanied by infection.
- Fever, chills, or flu-like symptoms
- Heavy postpartum bleeding, soaking a pad in under an hour
Emotional and Social Support
Mom-guilt is real, and emotional and social support may look a bit different for exclusively bottlefeeding parents.
First and foremost, it’s important to remember that your newborn’s wellbeing is directly connected to your wellbeing. A mother who is healthier, confident and more rested because she chooses not to nurse is giving her baby an enormous gift. At the same time, there are many reasons a mother can’t breastfeed ranging from illness, past trauma, taking medications that are contraindicated in breastfeeding or previous surgeries that make nursing impossible. Guilt may creep in in these situations but again, a parent who is healthy or trying to be, is a good parent.
If you’re faced with any shaming by others, set boundaries simply stating, “This is what works best for our family.” Surrounding yourself with supportive voices whether from friends, online groups, or other mothers who made similar choices can also help.
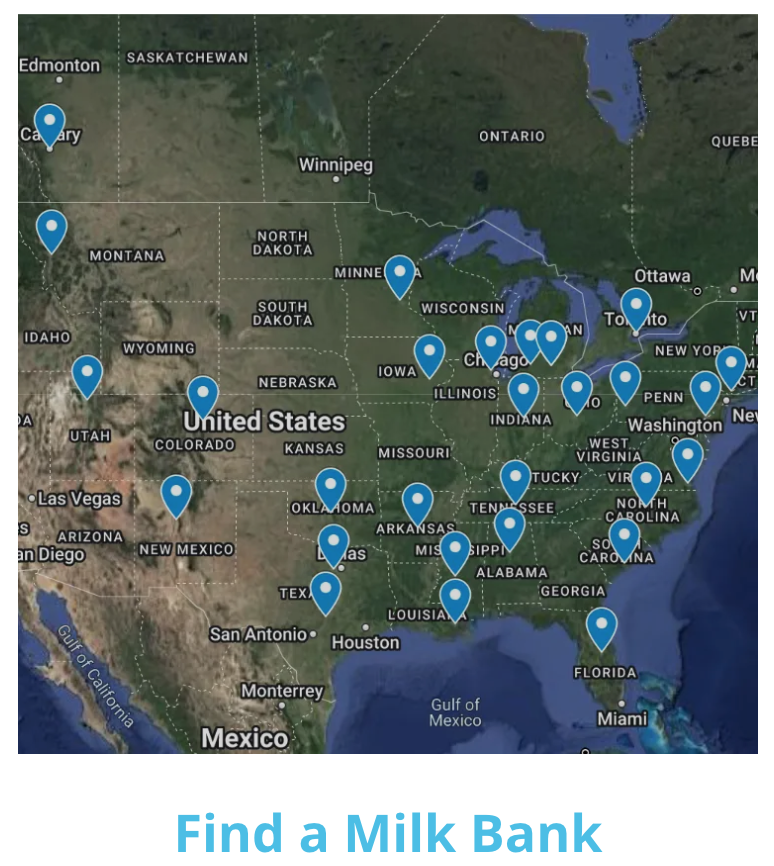
Postpartum Recovery: What if You’re Not Breastfeeding? – Donor Milk
Whatever the reason for not nursing, breastmilk is always available via donor milk banks. If this is something you choose to do, you can contact the Human Milk Banking Association of North America (HMBNA) for a donor bank near you, or so an online search for possible smaller, local donor milk banks.
Whatever infant feeding choice you make, postpartum recovery still involves breast comfort, hormonal adjustments, physical healing, nutrition and emotional support. Empowering yourself with these tips can make your early postpartum weeks safer and more comfortable.
If you’re expecting and liked Postpartum Recovery: What if You’re Not Breastfeeding?, sign up to receive our free newborn and postpartum email series!