Ultimate Guide to Baby Sleep Training
updated, October 23, 2025 – Written and medically reviewed by the Registered Nurse Advisory Board of Let Mommy Sleep
One of the most common questions our night doulas and newborn caregivers receive is: “Can you help our newborn get on a routine and sleep through the night?” It’s completely natural for parents to crave predictability after their baby arrives. There isn’t one “right” way to help babies sleep, but there are evidence-based, gentle methods that support both infant development and family wellbeing.
That’s why we created The Ultimate Guide to Baby Sleep Training, so families everywhere can access practical, expert guidance.
TL;DR: Quick Start to Helping Your Infant Sleep through the Night
Want to skip to the essentials? Here’s the condensed version:
- Wait until baby is about 4 months old and 14 pounds, with pediatrician approval.
- Ensure baby’s environment follows safe sleep guidelines (flat surface, back to sleep, no weighted blankets).
- Consolidate feeds to daytime and gradually wean overnight feeds.
- Use a consistent bedtime routine and choose a gentle, structured sleep training method (like the Slingshot Method).
- Stay consistent for 10–14 days while tracking progress.
Should You Sleep Train?
For this guide, “sleep training” means helping your baby sleep at least 6 hours overnight without unnecessary waking or feeding.
This topic sparks strong opinions, and the fact is both sides are right!
- YES, you should comfort your baby and meet their needs.
- ALSO YES, it’s healthy for your baby to learn to sleep independently if that’s right for your family.
Maternal mood and overall family wellbeing improve when parents get uninterrupted sleep. In fact, maternal mood scales statistically significantly improved when moms and dads get sleep. And we know there’s a direct correlation between Sleep Deprivation and Postpartum Depression. In other words, in a time where many of us don’t have loved ones to help care for our little children, we have to be our own little Village. This means using tools like sleep training to help the whole family function in a healthy way.
Managing Expectations: When to Start Sleep Training
Every baby is different of course but in general, 4 months and 14 pounds is a good time to start sleep training a full term baby. Here’s why:
- because this is usually when baby has physically grown enough to be able to skip nighttime feeds; their stomach is big enough to hold enough calories to keep them feeling fuller, longer.
- they’ve developed the hormone melatonin which induces sleep.
The 4 month pediatrician visit is the ideal time to confirm readiness for sleep training. This way you get the pediatrician’s confirmation that baby is ready to begin.
NOTE: Yes, we all have that friend whose child started sleeping through the night earlier than 16 weeks! And that’s great! And you and your pediatrician might agree that sleep training earlier is fine…and that’s also okay!
What Should Not Happen When Sleep Training:
Don’t “Sleep Train” a Newborn – There’s no reason to let a newborn (baby aged 1 -3 months old) cry it out. Crying indicates a need. As Night Doula Erin says, Newborns don’t learn *not* to be hungry, uncomfortable or scared.
- Don’t let newborns “cry it out.” They’re not manipulating you. They’re adapting to life outside the womb.
- Frequent, on-demand feeding every 2–3 hours is normal and healthy.
- Avoid rigid routines – Unless medically directed (e.g., NICU grads, preemies, jaundice), newborns don’t need strict schedules. Your baby’s natural clock will emerge if you remain responsive to their hunger and sleepy cues.
If it feels like baby sleep is a battle, pause and reset. Following your baby’s cues is the foundation of every effective sleep plan.

Understanding Infant Sleep Development – Ultimate Guide to Baby Sleep Training
The 4 Stages of Sleep
Adults experience four distinct sleep stages, but newborns only have two. Newborns gradually develop the full 4-stage cycle around 3–4 months, as melatonin levels mature.
The 2 sleep stages newborns have are:
- Quiet Sleep (Deep Sleep) – restorative, growth-focused.
- REM (Active Sleep) – light sleep where the brain consolidates learning.
Knowing this helps parents catch the sometimes elusive “drowsy but awake” window; the optimal time to place baby in the crib. You can learn more about how the stages of sleep develop in The Four Month Sleep Regression Explained.
Sleep Cycles By Age
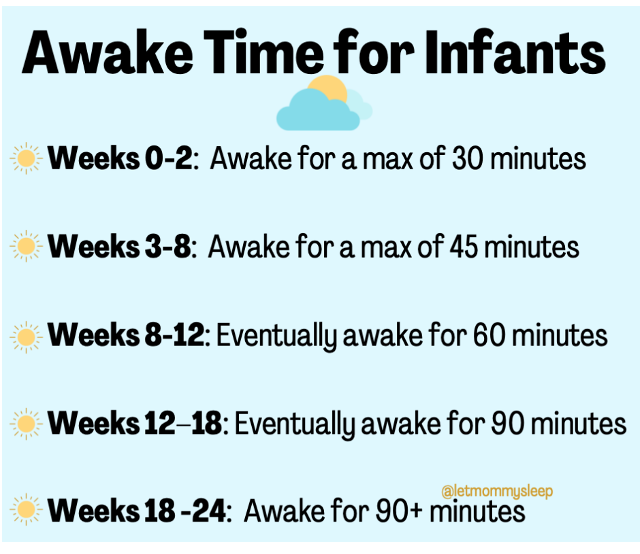
To help understand what’s expected in terms of baby sleep, here is a breakdown of newborns and infant basic awake and sleep times by age:
| Age | Awake Time | Sleep Notes |
|---|---|---|
| 0–2 weeks | 30 mins | Sleepy newborn stage; most awake time spent feeding. |
| 3–8 weeks | 45 mins | Baby more alert; white noise and babywearing can help. |
| 8–12 weeks | 60 mins | Melatonin still developing; short naps are normal. |
| 12–18 weeks | 90 mins | Begin longer awake periods and fewer naps. |
| 18–24 weeks | 90+ mins | Consistent naps form as baby nears 6 months. |
And here is a more in depth description of what’s typical each week:
- Weeks 0-2: Baby is awake for a maximum of 30 minutes. This is the sleepy newborn stage where most of your newborn’s time awake is spent feeding. You might even have to prompt them to try to wake up during a feed.
- Weeks 3-8: Awake for a maximum of 45 minutes. You’ll notice baby is more alert as they approach week 8. White noise, babywearing and giving a pacifier to help your baby sleep are all fine to do because at this age, your help to get and stay sleep is truly needed.
- Weeks 8-12: Baby’s awake time is eventually 60 minutes. You might need to help your newborn with napping if they wake up after 10-15 minutes by giving a pacifier or patting. Please know you’re not instilling bad habits. It’s developmentally appropriate that your baby needs a little help because the system that makes melatonin is not mature yet.
- Weeks 12 – 18: We’re getting to the 90 minutes of awake period! Baby is even more alert and may need help getting and staying asleep. Remember it’s okay to allow baby to play independently in the crib as long as they are happy. If you want them to sleep through the night eventually, there’s no need to rush them out of the crib when they wake up if they’re happy there.
- Weeks 18 -24: Your infant is awake for 90+ minutes and you’re seeing longer and fewer naps. Naps will vary in length, especially if you’re out and about during the day. If you’ve begun nighttime sleep training these naps become even more consistent.
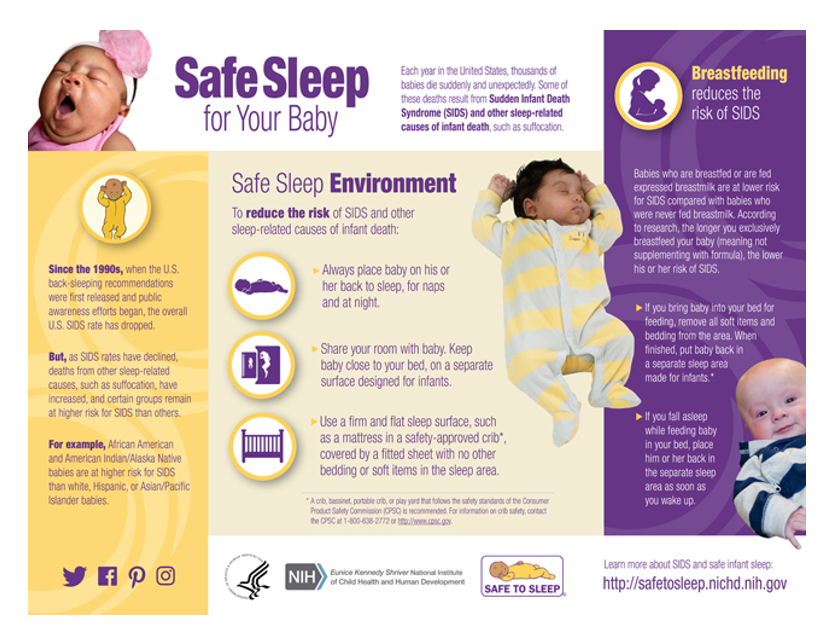
Safe Sleep: Reducing the Risk of SIDS
Before sleep training begins, ensure baby’s sleep setup meets AAP Safe Sleep Guidelines. Always place babies up to age 1 on their backs to sleep, alone on a firm flat mattress. This is true for naps as well as overnight sleep. You can read more in 10 Steps to Safe Sleep for Baby Please note that the AAP also cautions against using weighted swaddles and weighted sleep sacks on or near baby, as they are not safe and not recommended.
Steps to Sleep Through the Night
Now that we’ve addressed when to sleep train and how to make sure infants are in a safe sleep environment, we can move on to help baby sleep through the night.
There are 4 basic steps to sleeping through the night:
- Confirm with your pediatrician – Ensure baby is developmentally ready to sleep 6+ hours without feeding. As our night nanny team often reminds parents, this is important because you want to baby set up for success, but also because you will feel confident that you’re making the right decision.
- Consolidate daytime feeds over the course of about a week-
- Offer 4 daytime feeds of 6–7 oz every 4 hours, plus one 10 PM dreamfeed.
- Gradually space out feeds by 10–15 minutes each day until reaching 4-hour intervals.
- Wean overnight feeds at the same time you’re increasing daytime feeds:
- Reduce bottle size by ½ oz every 2–3 nights.
- Replace comfort feeding with a pacifier or gentle soothing as best you can
- Once night feeds are eliminated, you can begin formal sleep training.
- implement formal sleep training using the Slingshot Method
- The Slingshot Method, developed by Let Mommy Sleep, is a gradual, in-room approach:
- Night 1–2: Stay beside the crib and soothe with voice or touch.
- Night 3–5: Move slightly away; use voice only.
- Night 6–10: Sit near the doorway until baby falls asleep independently. Consistency and remaining calm are key. The goal is to shift from “I get help to fall asleep” → “I can fall asleep myself.”
With 4 feeding sessions of 6-7 ounces plus a final dreamfeed, your baby is getting enough calories to sleep longer than 3 hours through the night. In other words, 28-32 ounces should be enough so your baby doesn’t wake out of hunger. Your baby might still wake because their body is used to waking every 3 hours, but having taken in about 30 ounces prior to sleep, you can be assured they’re not hungry.
A few notes about transitioning baby to a 4 hour feeding schedule:
Eating larger meals at predictable times means baby will also anticipate rest at predictable times. This is the natural transition to having a “night” and a “day” instead of the 24 hour schedule of eating a bit, sleeping a bit, eating a bit, sleeping a bit. As our night nannies and postpartum doulas like to remind parents: We’re not taking away ounces at night, we are simply repositioning them to be taken in during the day.
Upon waking in the morning, give as much milk as baby wants at feeding time. For the next feed, work on holding off for as close to the 4 hour mark as possible. THIS WILL BE A GRADUAL PROCESS and may take 1-2 weeks. We never want baby to get to a state of frenzied hunger so it’s recommended to hold off feeds for 3 hours and 10 minutes on these first tries, then work up to 3 hours and 20 minutes and so on. Just push the feeding time up by a few minutes each day as tolerated by baby.
You’ll see baby is able to go longer and longer stretches with each feed until after several days, they’ll be doing the larger 6/7 ounce feeds every 4 hours.
Once we know baby does not need to eat through the night, and of course there are no other physical ailments that are outside of your infant’s control waking them, we can help them sleep through the night.
The Dreamfeed Explained
Coined by The Baby Whisperer, a dreamfeed means gently feeding your sleeping baby around 10 PM to prevent middle-of-the-night hunger. The reason it’s recommended at 10:00 is because you are still awake but your baby hasn’t yet naturally awakened out of hunger.
Sample Dreamfeed Schedule:
- 7:00 PM: Baby’s bedtime feed
- 10:00 PM: Dreamfeed while baby sleeps
- 10:20 PM: Quick diaper change, back to bed
A dreamfeed works because it shifts baby’s natural hunger window closer to parents’ sleep cycle.
How do you do a Dreamfeed? If you gently touch the bottle or breast to your baby’s lips, they’ll instinctively begin to suck if they’re hungry and stop once they’re full. By giving this feed before your baby wakes up from hunger, you’re essentially topping them off so they can stay asleep through the time they would normally wake to eat. This “pre-emptive” feeding, often called a dreamfeed, helps everyone get a longer stretch of uninterrupted sleep.
Nurse’s Note: You can do quick diaper change after the feed too just to be sure your infant is comfortable and clean! Our night nanny and postpartum doula team loves using wipe warmers for the dreamfeed. A nice warm wipe can help keep babies calm. Why startle them awake with a cold wipe if you don’t have to?!
Why Does A Dreamfeed Work? Without a dreamfeed, a baby who typically feeds in the 7 PM hour may awakens naturally from hunger at midnight, 1 AM or 2 AM. Giving a feed in the 10:00 hour allows parents to head off this hunger and may allow baby to sleep longer, usually until 4 AM.
Sleeping Through the Night: The Wind-Down Routine
When we think about sleep training, we often picture those middle-of-the-night wakeups: it’s 1:30 AM, do you go in and soothe, or wait a few minutes to see if baby settles? In reality, successful sleep training starts at bedtime, not at 2 AM.
If your baby can fall asleep independently at bedtime, usually between 7:00 and 8:00pm, they’re far more likely to resettle on their own when they wake overnight. Starting at bedtime also helps you prepare mentally for the process and be more patient, rather than being caught off guard in the dark.
To encourage self-soothing, establish a consistent 20–30 minute wind-down routine that happens the same way every night. Two or three predictable, calming steps signal to your baby that it’s time to rest.
A common sequence is: Bath → Bottle/Breast → Books → Bed.
This repetition helps your baby reach that “drowsy but awake” state where they’re tired enough to sleep, but still aware of being placed in the crib. That’s when the learning happens.
At this point, your baby will learn to fall asleep without being rocked, fed to sleep or relying on a pacifier. These are parent-managed sleep associations. When babies learn to manage their own falling-asleep process, they can also use those same self-soothing skills to return to sleep naturally during night wakings without needing help from you.
Ultimate Guide to Baby Sleep Training – What Method?
There are lots of sleep training methods out there but they all have one thing in common; the parent eventually cannot intervene. Sleep training or sleep coaching as it’s sometimes called, usually involves crying as a transition from being awake to asleep and each method essentially comes down to where you want to be positioned to hear the baby cry. Next to the crib? (The pick up/put down technique) In the hall? (cry it out) Popping in every few minutes? (Ferber).
None are right or wrong, we’re just making the point that sleep training methods aren’t really all that different from your baby’s point of view.
The formal sleep training technique our night nurses use is the Slingshot Method where you stay in the room while baby learns to go to sleep. You may choose another method at this point though and that’s fine! The important part is that the path has been properly laid so you know baby isn’t waking from hunger or something else outside of their control.
The Slingshot Method of Sleep Training
The Slingshot Method is a gentle, gradual approach to sleep training that helps babies learn to fall asleep independently while still feeling supported and secure.
During the first few nights, stay close to the crib and offer comfort through your voice or gentle touch. Patting, soft singing, or using the familiar “shhhh” sound can be reassuring—but try not to pick your baby up. The goal is to show that you’re nearby, while allowing your baby to discover how to fall asleep on their own. If it helps you relax, it’s fine to sleep in the same room for the first few nights.
Crying is expected, especially during the first few nights or if this is the baby’s first time without a pacifier. It’s common to hear 7–10 minutes of crying before they begin to settle. If crying escalates after about 10 minutes and seems to worsen, it’s perfectly okay to pause the session and try again later that night.
Over the next few nights, move gradually farther away from the crib—first across the room, then near the doorway. Continue to soothe with your voice, waiting slightly longer each time before responding. Eventually, you’ll be able to leave the room entirely. The goal is a steady transition from “I get help to fall asleep” to “I can do this on my own.”
If your baby wakes between 10 p.m. and 5 a.m., wait about 5–7 minutes before responding. Once babies can fall asleep independently at bedtime, they can usually soothe themselves back to sleep during night wakings. If you do check in, keep it brief and avoid picking them up; a calm voice or gentle touch is enough reassurance.
Most babies’ natural wake-up time is between 5:00 and 6:00 a.m. While this may feel early, it’s developmentally normal. If your baby wakes happy and alert, there’s no need to rush in right away. Letting them play or babble in the crib for a few minutes promotes independence and helps them associate the crib with calm and comfort.
If this isn’t ideal, just remember that it’s not forever. Also- you don’t have to go rushing in to get your baby simply because they’re awake. If they are babbling or trying to scoot around the crib in the morning, it’s perfectly fine and healthy to let them play independently as long as they are doing so happily. After all, we want the crib to be somewhere they look forward to being!
Consistency is Key
The single most important factor in successful sleep training is consistency. Once you’re confident your baby isn’t hungry, teething, or unwell, sticking with your chosen method allows your baby to learn faster and with less confusion.
For example, if your baby cries for 10 minutes and is then given a bottle, they quickly learn that “crying for 10 minutes = bottle.” This resets progress and reinforces the behavior you’re trying to replace. Staying consistent—even when it’s hard—teaches predictability and builds your baby’s confidence.
Sample Sleep Schedules For Babies
Now that you understand how to guide your baby toward independent sleep, these sample schedules can help you picture how feeding and naps fit into a 24-hour rhythm. Here are All the Infant Sleep Schedules in One Place
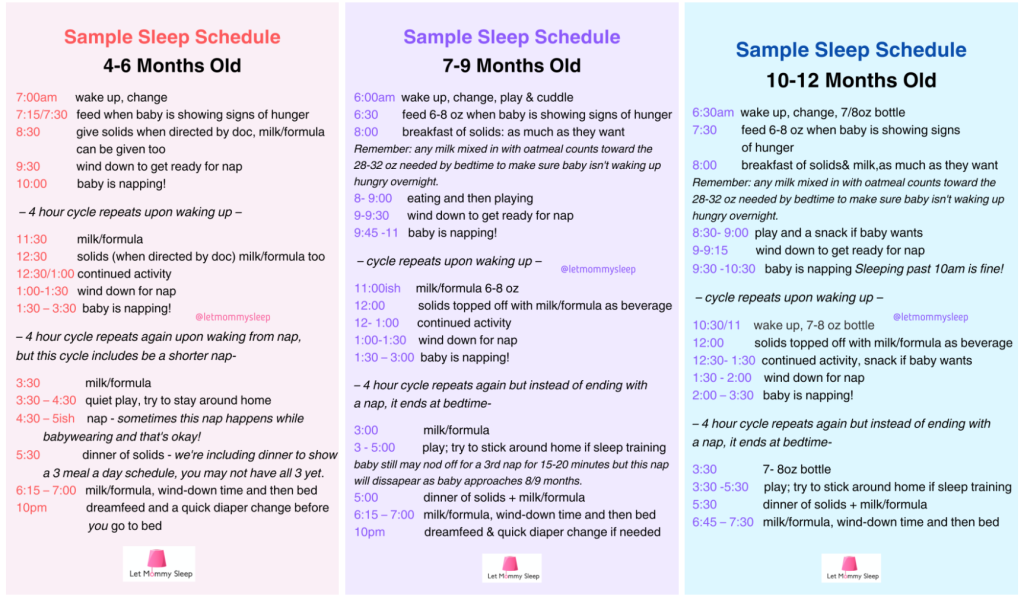
Things to remember about these Infant Sleep Schedules:
– These are examples only. Every baby and family is different, and it’s fine if your schedule looks different or if you don’t follow one at all.
– The purpose of a schedule is simply to help establish consistent start and end points to each day, creating space for one long stretch of overnight sleep.
– Use your baby’s actual wake-up time to adjust any example schedule.
– Around 7–8 months, babies often drop their late-afternoon nap (around 4:00 p.m.), which is a normal part of consolidating sleep.
Ultimate Guide to Baby Sleep Training – The Four Month Sleep Regression
The “Four-Month Sleep Regression” is a normal developmental phase, not a setback. As we talked about above, newborns initially experience only two sleep stages: deep sleep and REM and around three to four months, the brain reorganizes to include all four sleep stages, just like adults.
When this change happens, REM sleep decreases from about 50% to 25% of total sleep, making room for lighter sleep stages. This means your baby is now more likely to wake up during the night—but that’s completely normal. Even adults wake up multiple times per night; we just don’t remember it.
What you can do to help your little one through the 4 Month Regression
- Darkness: Babies aren’t afraid of the dark; they’re simply responsive to light. Keep sleep environments dark to encourage melatonin production and restful sleep.
- White Noise: Light sleep means more chances to wake from sudden noises. White noise helps mask environmental sounds.
- Bedtime Routine: Continue a 20–30 minute calming routine like bath, bottle/breast, books then bed placing your baby in the crib drowsy but awake.
Once again, our night nanny and postpartum doula team recommends talking to your pediatrician at the 4 month well check is so baby can get through this regression before formal sleep training. You’ll get reassurance that they’re now ready to follow the sleep patterns they’ll have for the rest of their lives.

Troubleshooting Common Infant Sleep Issues
Will adding rice cereal to the bottle help baby sleep longer?
No. Studies, including those from the NIH, show no relation to thickening formula and longer sleep. Thickened formulas are used only under medical guidance for specific conditions.
My baby has gas, how can I help?
Offer slow feeds with frequent burping, keep your baby upright for at least 30 minutes after feeding and try gentle tummy massage or bicycle kicks. Ask your pediatrician about probiotic options to support gut health.
Why does my baby wake at night if they’re not hungry?
Common reasons include: discomfort from congestion or ear infection for example, teething (typically between 4–7 months), or simply following the same 3 hour cycle they do during the day. Once cleared by your pediatrician, gentle night weaning can help break the cycle of waking.
When should I stop swaddling?
Stop swaddling once your baby starts rolling. Transition gradually by freeing one arm and then the other while keeping gentle pressure on the abdomen. Learn How to Swaddle Like a Pro
How do I reduce or stop overnight feeds?
Wean slowly by decreasing one-half ounce (or a few minutes of nursing) from each night feed. You can give a pacifier after giving the smaller amounts of milk if baby needs to suck to feel soothed.
What about the pacifier itself?
Gradually shorten pacifier time during bedtime or remove it once sucking stops or slows. If you prefer, you can go “cold turkey,” but the gradual method is often easier for both baby and parent.
How do I sleep train for naps?
Once your baby is successfully sleeping through the night there is no special “nap training” that has to happen. One big caveat though: Naps can be inconsistent for so many reasons: your own family schedule, unexpected trips out of the house and the many gradual transitions babies make in growth.
My toddler still wakes up. What can I do?
Toddlers often test boundaries or crave reassurance. Keep routines consistent and calmly return them to their bed each time. They’ll learn the new pattern through repetition. Learn more in Sleep Coach Your Toddler
The Bottom Line
Whether you’re dedicated to following an infant sleep schedule or you’re out and about without a schedule, there are a lot of ways to keep your newborn, infant and older kids happy and healthy. As long as your family is safe, harmonious and healthy, the parenting you’re doing is right.
Even if you follow expert advice exactly as it’s written, your newborn, infant and toddler will still cry. They will cry to a point where you might experience frustration that scares you. If this happens it is okay to put your baby down in the crib or other safe space and walk away for 15 minutes. You can go back in when you’re more calm. And maybe your child is more calm too. If you’re concerned about baby’s crying or health, please contact your pediatrician.
Our infant sleep plans were written by Registered Nurses and Night Nannies using the guidance of our Medical Advisory Board. They’re not intended to be used as or replace medical advice. Any kind of sleep training or change to your baby’s feeding and sleep habits should only happen under the direction of your child’s primary care physician.
If you’re struggling emotionally, please reach out to 1-833-TLC-MAMA. You can also learn more in PPD vs. Baby Blues: Know the Difference.
If you’re expecting and want more tips, read Your First Week Home with Baby: Ultimate Q&A our newborn and postpartum support guide!
Categories
- Corporate Care & Partners
- COVID19 Archive
- En Espanol
- Expert Guides
- Hiring a Night Nanny
- Infant Safety
- Infant Sleep Hub
- Newborn Care
- Postpartum Health
- Twins & Multiples
- Work as a Night Doula
- zPost Archives
