My Milk Isn’t In…What Do I Do?
updated, Sept 1, 2025 – Jessica Haupt, RN, BSN, IBCLC provides answers to nursing with low production, or what seems like low-production but is actually quite normal! Tips on increasing your milk production and a successful breastfeeding relationship are below in My Milk Isn’t In…What Do I Do?

One of the challenges you might encounter just home from the hospital is what feels like a lack of milk production. While this is normal, you should know that frequent breastfeeding where it seems like “nothing is coming out” is typical as milk comes in Of course we want to be sure baby is gaining weight and satisfied after feeds as well and there are things you can do to be sure your newborn is okay.
My Milk Isn’t In…What Do I Do?
- Remember that days 3-5 are the hardest. I get the most calls during these days. Babies get hungrier and milk can often be delayed until day 5. There are many reasons for delayed milk, but the most common seem to be c-section, complicated delivery or obesity.
- Have someone take care of YOU, so YOU can take care of feeding the baby. Stress, hunger and sleep deprivation delay lactation even more. Friends and family can be overwhelming, but it’s important to have someone whose job is to look after you. They need to be sure you’re eating, drinking and resting. (Not adding more work!)
- No time at the breast is wasted time. By the same token, no drop of colostrum or milk is wasted. The benefits of breast milk can be transferred to baby drop by drop, even if the baby is primarily getting nutrition from formula. Every bit of milk you can give your child, even if it seems like a small amount, is a benefit to the baby’s health. And remember, baby’s belly is only the size of a walnut to an apricot on days 3-7.
- Sleep when you can – As many studies report, Collected milk volume was strongly positively correlated to stage N3 sleep duration. Expressing milk is still important but restorative sleep aids healing and milk production.
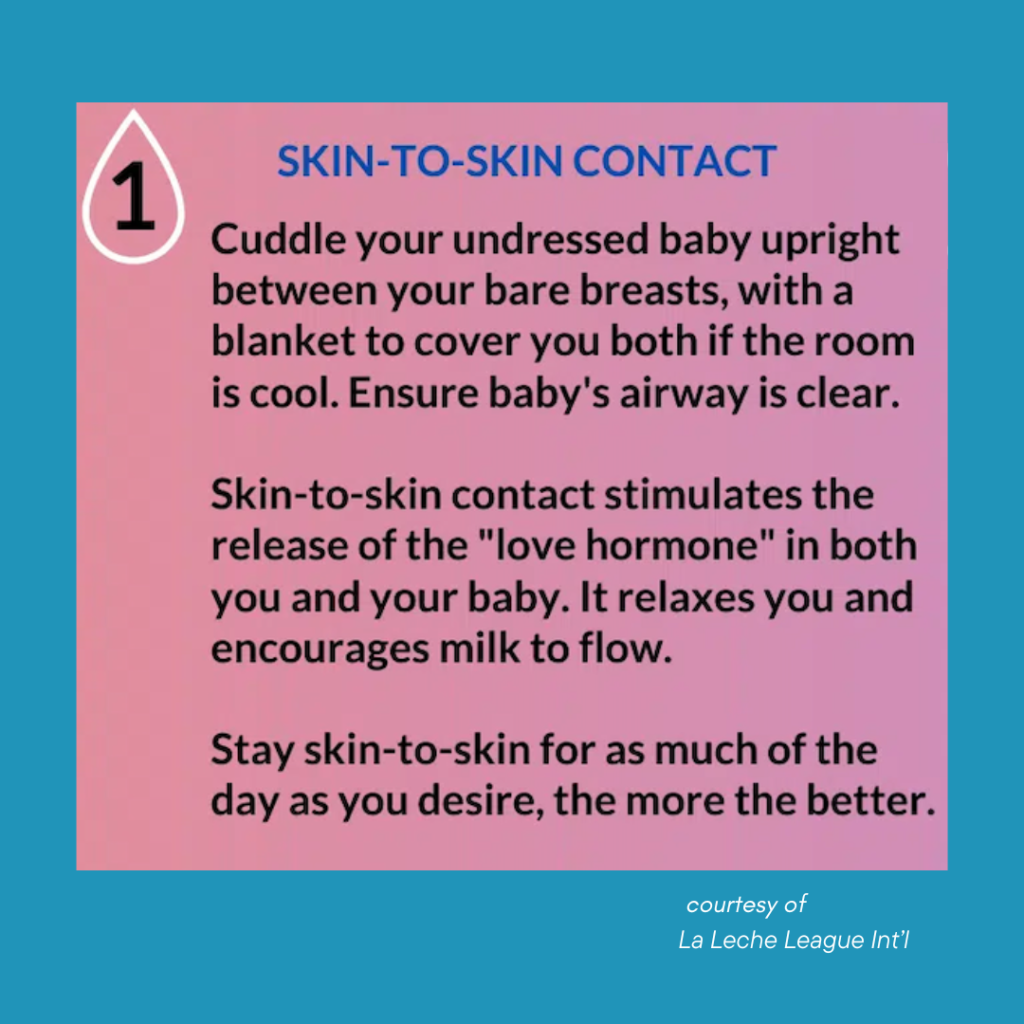
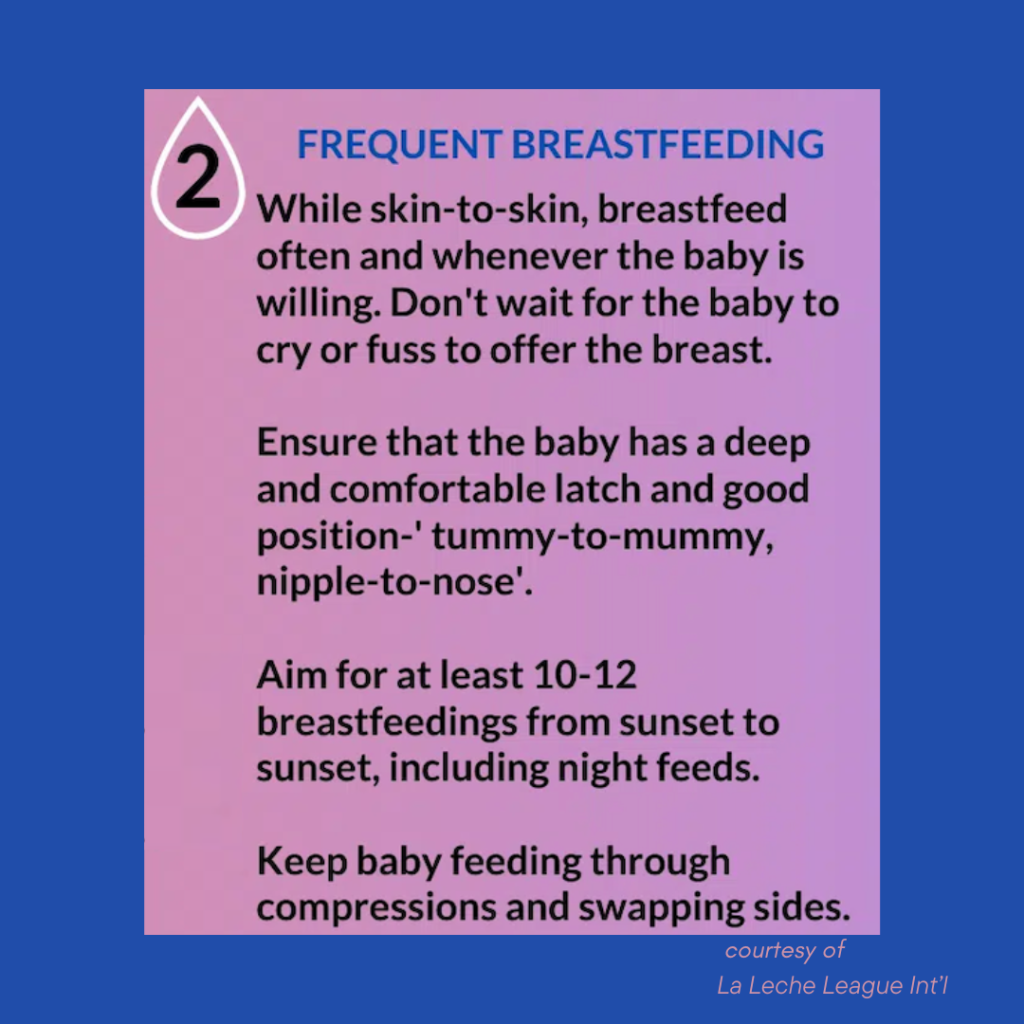
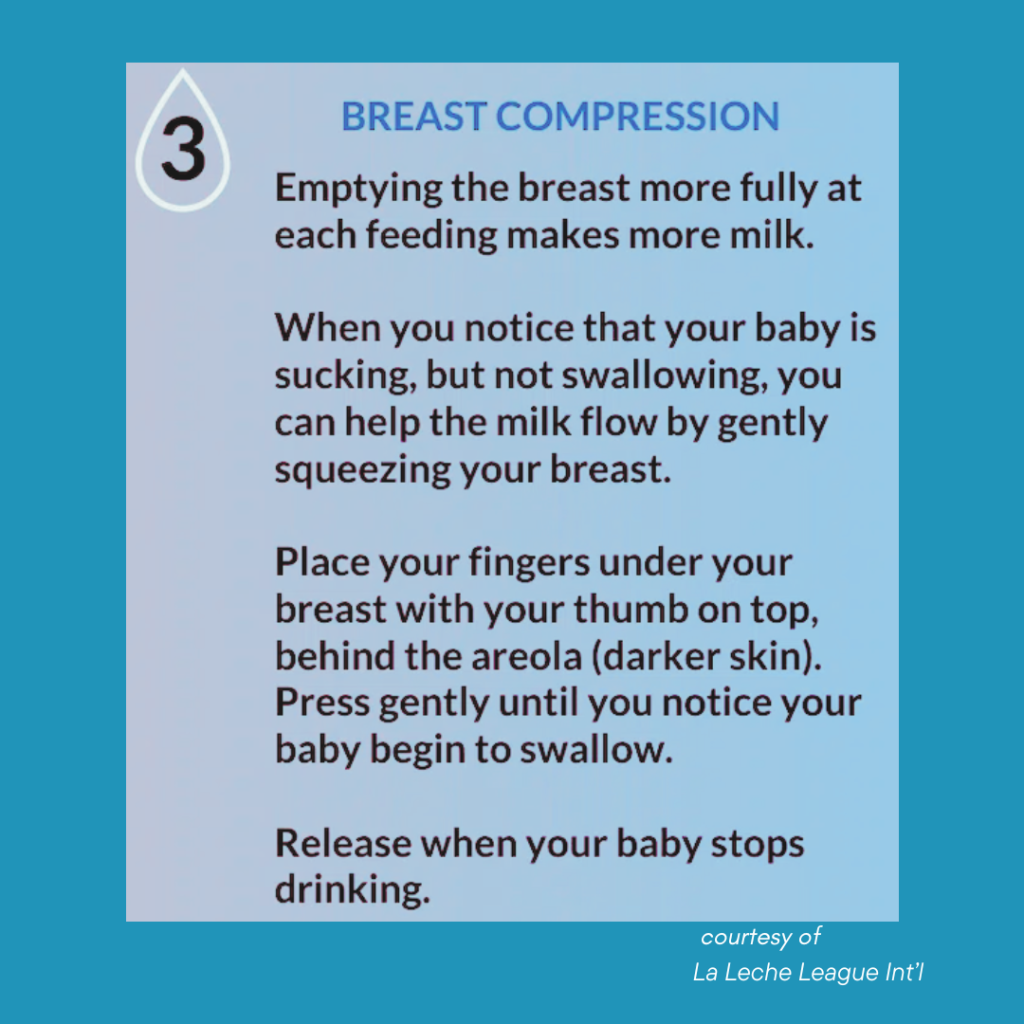
Helping Milk to Come in is as Easy as 1-2-3!
What Else Can I Do if My Milk Isn’t In?
- Don’t wait until baby is screaming angry to put the baby to the breast. Learn the early signs of hunger and put the baby skin to skin with mom before latching. Non-feeding caregivers should also learn the signs of hunger. That fresh set of eyes if you’re too tired can make a huge difference.
- Skin to skin works! The World Health Organization,(WHO) found that: 90 minutes of uninterrupted skin-to-skin contact after birth, maximizes the chance for your baby and you to be physically ready to breastfeed.
- Skin to skin is for dads and partners too! Additionally, dads and partners also benefit from the intimacy of skin to skin while helping baby grow and get stronger.
- Check your latch If your nipples are sore, reach out to lactation consultants, La Leche, or your birthing center or hospital for resources and to get a latch check.
- Utilize the benefits of hand expression! In the early days, you may find hand expression more productive than pumping. Good hand expression can be used during nursing as well and can help stimulate let down. Stanford has a great video on this.
What if I do All That and Breastfeeding is Still Not Working?
If all else fails and you’re just not producing, consider alternative methods of supplementation other than a bottle while waiting out until days 5-7, when lactation usually onsets. Spoon or cup feeding formula can be used. A needle-less syringe can be used for finger feeding. Supplemental systems like those by pupolar brand Medela with a nipple shield can keep the baby nursing while also promoting breastfeeding.
And finally – I end with a quote from a wonderful midwife that I know: “Formula is not the devil’s spit”. While breast is best, a baby who is screaming from hunger is a baby that needs to be fed. Listen to your pediatrician – if the baby is not making enough wet diapers, losing or not gaining weight, supplementation is necessary and does not mean that breastfeeding is over forever.

My Milk Isn’t In…What Do I Do? – How Can I Get More Breastfeeding Help?
Private Lactation Counselors – Jessica Haupt who wrote this article, is a Registered Nurse with a Bachelor of Science in Nursing and an Internationally Board Certified Lactation Consultant (IBCLC). You can find a lactation counselor by asking your pediatrician, hospital or birthing center or us!
Video Help – Check out the International Breastfeeding Centre’s excellent library of resources.
LLL – We also love La Leche League for support and evidence-based information and to answer the question, My Milk Isn’t In…What Do I Do?
If you’d like to learn more about what to expect during the first weeks home with your baby, read Your First Week Home with Baby: Ultimate Q&A.
Categories
- Corporate Care & Partners
- COVID19 Archive
- En Espanol
- Expert Guides
- Hiring a Night Nanny
- Infant Safety
- Infant Sleep Hub
- Newborn Care
- Postpartum Health
- Twins & Multiples
- Work as a Night Doula
- zPost Archives
